Titan Arm
Month
We’re pleased to announce that we’ve been accepted to the Cornell Cup Competition! Cornell and Intel have teamed up to present an embedded systems competition. We’ll be competing this May is Disney World, Florida! Stay tuned.

Based on our actuation selection, a cable drive will be implemented on the exoskeleton to transmit the power from the motor to the elbow joint. A cable drive system allows for non-localized actuation. Other exoskeletons, such as HAL (image below), use localized motors for actuation. With non-localized actuation, it is possible to increase the motor strength and decrease the weight at the joint extremities.
We’ll be investigating cables and sheathing to transmit the force from the back to the elbow joint.
After months of deliberation, our team decided to purse an actuated upper body exoskeleton for use in the fields of healthcare, search and rescue, and strength intensive occupations.
Isolating simply the actuation subsystem, our team researched four different forms of actuation:

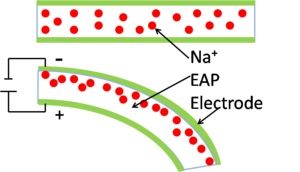

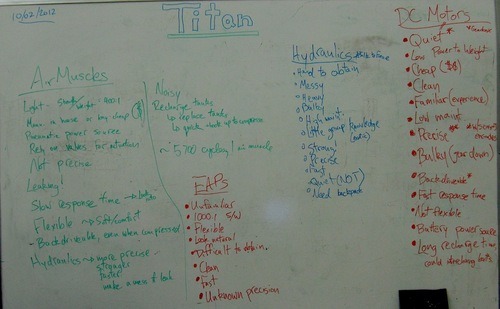
Fig. 1: Our whiteboard brainstorming session.
Our team has decided to move forward with a DC motor actuation system. This system was chosen because the team has experience; DC motors are already relatively inexpensive, clean, quiet, and precise.
One way of creating a natural user experience is to give a quick, smooth response to the user input. This is no small feat; how can you tell when a user requires additional strength? Electromyography is a potential solution. Electromyography, or EMG, is a way of sensing muscle activity through electrical signals. When muscles are activated by the brain, an electrical potential can be measured in the range of 50uV to 30 mV. By amplifying and filtering the signals, it’s possible to read and decompose the signals. When the muscles are inactive, the electrical potential is low; however, when lifting an object, the electrical potential rises. As the work required of the human increases, more muscle is called on to help lift the object, increasing the potential even higher. Therefore, using the correct sensors and filtering, it’s possible to scale the amount of aid from an exoskeletal suit.
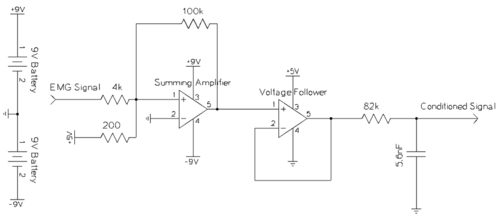
Figure 1: The circuit used for amplifying and filtering EMG sensor data.
One of the team members’ brothers, Steve McGill, worked on a project with EMG sensors a few years back for his senior design. We enlisted his help in developing a EMG solution and borrowed his circuit, still working after three years of inactivity (Fig. 1). The sensors he lent us were high quality collocated EMG pads (see Fig. 2). This setup was found to be a “binary” approach, capable of determining if there was any muscle activity or none at all. This result was exciting, especially so early on in our project, but not ideal. An ideal signal would clearly represent a gradient of muscle activity, delineating both small and large loads. Luckily, a little digging online led to some interesting circuits that we’ll be investigating soon!

Figure 2: Two EMG sensors. These were applied directly to the skin and attached with typical bandage wrap.
The transition from no assistance to assistance could be triggered with these EMG sensors, but it’s not clear yet how to stop the external support. For example, when lifting a heavy box, the assistance could be triggered once the EMG signal crosses a certain threshold. This would allow the user to lift the box in a continuous angular rotation. However, a trigger must be set at the desired arm angle to lock the user’s arm in place. Current systems use an external controller to actuate and stop the user’s motion; it would be ideal to encapsulate the system and localize control to the user.

In order to get a better grasp of the applications of our project in physical therapy, our team met with Jennifer Dekerlegand, a physical therapist at the Hospital of the University of Pennsylvania (HUP). Jennifer has worked with engineers at Penn before and has a thorough understanding of the world of physical therapy. The biggest takeaway from our meeting was that developing the strength of the patient is much more important than developing the range of motion. To that end, we’ve put an emphasis on strength development in our design plans.
Jennifer will be a knowledgeable resource as we continue to develop and refine our project scope. Already, she’s helped us rule out the use case of a nursing assistance exoskeleton – such a device would be work than it’s worth. She’s also given us personal stories interacting with the Ekso Bionics lower body exoskeleton and the positive impacts on the patients.
Our team is designing an untethered, powered, upper body exoskeleton for use in the fields of rehabilitation and therapeutic application, as well as occupations requiring augmented strength. Though systems exist, past exoskeleton endeavors have led to bulky, expensive, invasive, and tethered solutions. The challenge is to build an exoskeletal system that is inexpensive, streamlined, and wireless.
Our solution is unique in that it will be a low-cost, ergonomic device actuated through sensors measuring the user’s motion and muscle activity. Through onboard sensing, the skeleton can provide rich data, such as range of motion or strength for use in physical therapy. This data can be used by doctors and patients to more accurately track improvement over time. With its low cost, hospitals could employ multiple devices and aid a larger audience of patients; the devices could even be used at home for physical therapy, which would dramatically increase quality of life for patients.
Outside of physical therapy, augmented strength is applicable to physically intensive occupations, as well as search and rescue operations. Each year, thousands of workers must take leave due to injuries triggered by heavy lifting; with augmented strength, workers could avoid harmful situations.
